10 Warning Signs of Diabetic Retinopathy You Shouldn’t Ignore
Diabetic retinopathy is a serious eye condition that affects many individuals with diabetes. Recognizing the warning signs early can be crucial in preventing severe vision loss. In this article, we will explore the ten warning signs of diabetic retinopathy you shouldn’t ignore, along with insights into diabetic retinopathy treatment, living with diabetic eye problems, and maintaining overall eye health.
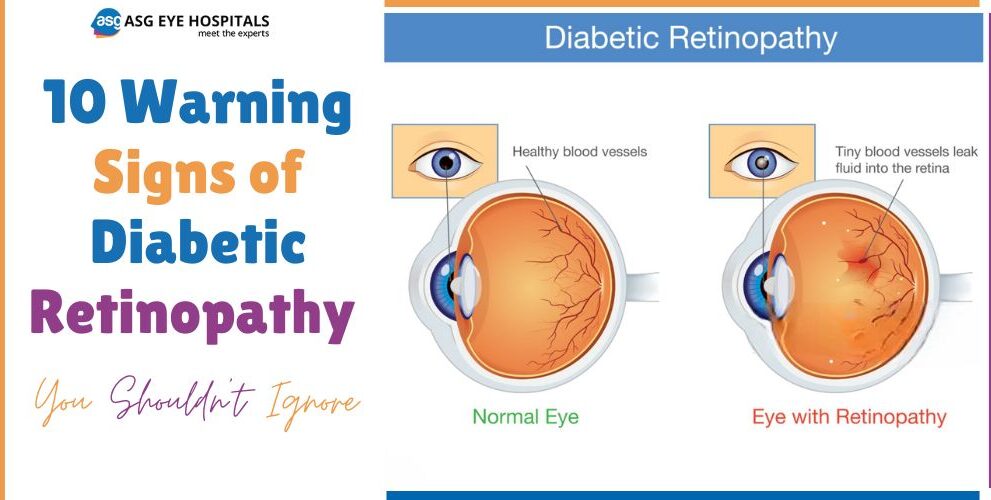
What is Diabetic Retinopathy?
Diabetic retinopathy is a complication of diabetes that occurs when high blood sugar levels cause damage to the blood vessels in the retina. The retina is the light-sensitive tissue at the back of the eye that is essential for vision. There are two main types of diabetic retinopathy:
- Non-Proliferative Diabetic Retinopathy (NPDR): Early stage where blood vessels in the retina weaken and may leak fluid or blood.
- Proliferative Diabetic Retinopathy (PDR): Advanced stage where abnormal blood vessels grow on the retina, leading to severe vision problems.
Why You Should Be Concerned About Diabetic Retinopathy
Diabetic retinopathy is a leading cause of blindness in adults. The impact on vision can be profound, affecting daily activities and quality of life. According to the Centers for Disease Control and Prevention (CDC), nearly one-third of diabetics over the age of 40 have signs of diabetic retinopathy.
Warning Signs of Diabetic Retinopathy
Blurred Vision
One of the earliest signs, blurred vision, can occur due to swelling in the retina’s blood vessels. This symptom might come and go, making it easy to dismiss.
Floaters and Dark Spots
Seeing floaters or dark spots is another common symptom. These can be small pieces of debris floating in your field of vision, caused by bleeding into the eye from damaged blood vessels.
Fluctuating Vision
Frequent changes in vision clarity can signal diabetic retinopathy. This happens when blood sugar levels fluctuate, affecting the eye’s focusing ability.
Impaired Color Vision
Difficulty distinguishing colors or noticing that colors appear faded can indicate damage to the retinal blood vessels.
Dark or Empty Areas in Vision
Experiencing dark or empty patches in your field of vision can be a sign of severe damage to the retina, requiring immediate medical attention.
Sudden Vision Loss
Abrupt loss of vision is a serious warning sign and can result from a vitreous hemorrhage or retinal detachment, both requiring urgent intervention.
Difficulty Seeing at Night
Night vision problems can occur due to poor blood flow to the retina, making it harder to see in low-light conditions.
Seeing Halos Around Lights
Seeing halos or rings around lights is another indication of potential retinal damage.
Poor Central Vision
Loss of sharp central vision, necessary for tasks like reading and driving, can be a symptom of diabetic macular edema, a complication of diabetic retinopathy.
Eye Pain or Pressure
Although less common, eye pain or a feeling of pressure can occur with advanced stages of diabetic retinopathy and may signal an increased intraocular pressure.
Understanding the Severity: Non-Proliferative vs. Proliferative Diabetic Retinopathy
Non-Proliferative Diabetic Retinopathy (NPDR): This stage involves microaneurysms, retinal hemorrhages, and fluid leaks causing retinal swelling.
Proliferative Diabetic Retinopathy (PDR): This severe stage involves new, abnormal blood vessel growth, leading to vitreous hemorrhage and possible retinal detachment.
Diagnosis of Diabetic Retinopathy
Comprehensive Eye Exam
A thorough eye exam can reveal early signs of diabetic retinopathy.
Dilated Eye Exam
This involves using drops to widen the pupil, allowing a detailed view of the retina.
Fluorescein Angiography
A special dye is injected into the bloodstream, highlighting the blood vessels in the retina.
Optical Coherence Tomography (OCT)
This imaging test provides detailed cross-sections of the retina, revealing areas of thickening or swelling.
Diabetic Retinopathy Treatment Options
Laser Treatment
Laser surgery can seal leaking blood vessels and reduce retinal swelling.
Vitrectomy
This procedure removes blood from the vitreous gel in the eye, improving vision.
Medication Injections
Anti-VEGF injections can reduce abnormal blood vessel growth and fluid leakage.
Lifestyle Changes
Maintaining healthy blood sugar, blood pressure, and cholesterol levels through diet and exercise can slow the progression of diabetic retinopathy.
Preventing Diabetic Retinopathy
Maintaining Blood Sugar Levels
Keeping blood sugar levels within the target range is crucial.
Regular Eye Exams
Annual eye exams help detect changes early.
Healthy Diet and Exercise
A balanced diet and regular exercise support overall eye health.
Managing Blood Pressure and Cholesterol
Controlling these factors reduces the risk of diabetic complications.
Living with Diabetic Eye Problems
Coping Strategies
Using magnifying glasses, brighter lighting, and large-print materials can help.
Support Systems
Joining support groups and seeking counseling can provide emotional and practical assistance.
Technological Aids for Vision Impairment
Devices like screen readers and talking clocks can improve quality of life.
Importance of Regular Eye Exams
Frequency of Exams for Diabetics
Diabetics should have a comprehensive eye exam at least once a year.
What to Expect During an Eye Exam
Expect tests like visual acuity, dilated eye exam, and retinal imaging.
When to See a Doctor
Recognizing Urgent Symptoms
Seek immediate medical attention for symptoms like sudden vision loss or eye pain.
How to Prepare for Your Visit
Bring a list of symptoms, medications, and questions to discuss with your doctor.
Potential Complications if Ignored
Ignoring diabetic retinopathy can lead to blindness and increase the risk of other eye diseases such as glaucoma and cataracts.
Personal Stories and Testimonials
Real-life experiences highlight the importance of early detection and treatment. These stories often underscore the impact of proactive care and regular monitoring.
FAQs About Diabetic Retinopathy
Q1: Can diabetic retinopathy be reversed?
A1: While it can’t be reversed, early detection and treatment can prevent progression.
Q2: How often should I get my eyes checked if I have diabetes?
A2: It’s recommended to have a comprehensive eye exam at least once a year.
Q3: What lifestyle changes can help manage diabetic retinopathy?
A3: Maintaining healthy blood sugar levels, a balanced diet, regular exercise, and managing blood pressure and cholesterol are essential.
Q4: Is diabetic retinopathy treatment painful?
A4: Treatments like laser surgery and injections may cause discomfort, but they are generally well-toler

 English
English 



